Chris Buck
Akiko Iwasaki knows how to listen. She listens with the kind of intensity that makes a bustling room recede into the distance, leaving a quiet space around her and the one she’s listening to. When she speaks, it’s with a steady clarity, and her eyes stay with you, checking, watching, assessing. She’s a slender person with a big laugh and a placid, implacable sense of justice.
Before the pandemic, Iwasaki, a professor of immunology at the medical school, was well known for her elegant work on what happens when viruses like herpes and Zika pierce our defenses. With the pandemic, everything changed; she is now one of the foremost researchers studying the immune response to SARS-CoV-2. In 2022, she was made a Sterling Professor—Yale’s highest academic honor.
If reworking her entire lab at the beginning of the pandemic to study this new virus was stressful, there is little about her demeanor now to suggest it. One warm fall day in her office at the medical school, she chatted about new designs for vaccines and reporter Ed Yong’s Pulitzer Prize–winning coverage of the pandemic. She reflected on the moment onstage at Harkness Auditorium in February 2020, sitting next to her colleague Albert Ko, when the two scientists glimpsed what was coming.
“The virologists at Yale put together an informational session on this novel coronavirus; we didn’t have a name yet,” she remembers. “Albert and I just sort of sat there and thought, Oh, my God, this thing is huge.” The virus was looming. Ko had just enough time to set up the protocols and permissions required to collect samples from patients admitted to Yale New Haven Hospital before the first wave broke over them, and the old world was gone forever.
“I didn’t know at that time that this was going to become my life,” she says. But she’s always been someone who’s ready when new things come along—ready to take a chance.
Akiko Iwasaki, the oldest of three girls, was raised near Osaka in Japan’s Kansai region. She remembers a childhood spent playing in rice paddies, catching tadpoles, and reading Japanese literature. “I was not very studious as a young child,” she recalls. But she had a front-row seat to a struggle of epic proportions: in a society where women were discouraged from having careers after having children, her mother fought to keep her job at a large media company while she raised her daughters. Eventually, Iwasaki’s mother—considered a temporary worker throughout decades at the company—won recognition as a full employee. “I’ve seen some struggles,” Iwasaki says, “but through the struggle, I also learned from my mother’s example that you can really stand up for yourself and for others, to make the workplace a better place.” Iwasaki has been known to end an invited lecture by stumping for the need for good childcare—an essential, if we are serious about keeping women in science.
She grew enchanted with math, a passion that served her well when she accompanied her father, a physicist, on a sabbatical in Maryland. It was a strange time. “He didn’t know how to cook,” she says. “We ate fast food a lot.” And it was a difficult adjustment. Iwasaki still keeps in touch with the girl who helped her when she was stymied by the lock on her American-style locker. “I was just turning into a teenage girl, and thrown into a completely foreign country with foreign languages. But I survived.” A laugh burbles out of her, as she reflects on the absurdity of the whole thing. “I think what kind of made me survive is math,” she says, “because math is universal.”
After returning to Japan, Iwasaki grew uneasy with the future she saw there for herself. She decided that she didn’t want to be a housewife. At sixteen years old, she convinced her parents to let her move to Canada to finish high school, and then attended the University of Toronto. “I didn’t think I was going to stay in North America for life,” she says. She just wanted to see what she could do.
As the years passed, she fell in love with immunology and moved on to graduate school. Math and physics had nice, clean numbers, but immunology is a baroque, impossibly complex black box, a swarm of cells whose roles and identities seem to morph and shift to protect the host against invaders. “I just love the mystery of it,” she says. As a graduate student, she studied DNA vaccines, the precursors to the mRNA vaccines in use today, and she overturned a widely held theory about how they worked.
She found herself drifting farther and farther from the rice fields outside Osaka. “The more I pursued education and science,” she says, “the more I got hooked and the more remote the possibility of going back to Japan became, because the gap of what I could do here versus what I could do there was becoming so huge.” She thought, I’ll stay in North America as long as I can, and if I can get a job, I’ll stay longer.
“And so that’s how I ended up in this country,” she says. She moved to the United States for a postdoctoral fellowship at the National Institutes of Health. Two years later, in 2000, she was setting up her lab at Yale. She had decided to study infections in a tissue long neglected by science: the vagina. If she could understand how herpes simplex viruses—presently incurable and responsible for the silent suffering of half a billion people—evaded the immune system, then perhaps she could see a way to flush them out.
What do you do with a newly minted PhD and a lot of big ideas? Usually, you start learning new techniques and making connections as fast as you can, and Iwasaki was no exception. Having never worked with herpes viruses before, she jumped on Amtrak to Boston and asked David Knipe, a virologist at Harvard Medical School and an expert in the herpes viruses, to teach her how to work with them. “I was just, like, completely imposing—‘How do you do everything?’” she remembers. “He was very generous. After three trips to Boston, I was equipped.”
Over the next few years, she and her lab used mice to start mapping out what happens when herpes invades the vaginal mucosa—the soft tissue that lines the vagina. “We found so many amazing insights about how the virus is detected, what cell types are stimulating the immune response, and basically the time course, from the time of infection all the way to memory stage”: the stage when the immune system has produced cells that will recognize the virus if it’s ever encountered again. Along the way, she added more and more viruses to the lab’s portfolio of subjects. Each virus has its own strategy for escaping the immune system; each has something for the attentive observer to find. Her team even began studying the endogenous retroviruses—pieces of viral genetic material that crept into the human genome long, long ago.
Iwasaki grew interested in why vaccines for herpes had failed. For some viruses, a shot in the arm that provokes an antibody response is all that’s needed for protection. In those cases, memory cells will circulate throughout the body to keep infection away. But for viruses like herpes, it’s not enough. In a landmark 2012 paper, Haina Shin (then a postdoc in the lab) and Iwasaki discovered that if memory cells made by a standard vaccine could be lured from the bloodstream into the vaginal mucosa, mice became immune to infection. They applied two chemokines—chemical signals made by the cells of the immune system—to the surface of the mucosa, and watched as the memory cells answered the call, taking up permanent residence in the very tissue that herpes invades. They dubbed the strategy “prime-and-pull.” The shot primed the body to fight off herpes, triggering the production of memory cells, and the chemical signals pulled the cells to the place where they could do the most good.
The approach was elegant, powerful, and meticulously thought out. “It was a seminal piece of work,” says Mark Coles, a professor of immunology at the University of Oxford. He remembers the first time he read the paper; he knew he would be using it to teach fundamental concepts to his students for years. Coles notes that Iwasaki has a tremendous ability to take the complicated details of immunology, pluck out profound, universal concepts, and write about them in a way that sticks in the mind. “Brilliant science, communicated in an effective way—that’s Akiko,” he says.
Inspired by the 2012 paper, David Bernstein, a researcher at University of Cincinnati Medical School, and his colleagues took the work to the next level. They demonstrated in 2019 that guinea pigs that already had herpes infections could be prevented from suffering repeated flare-ups—and, crucially, from spreading the disease—if treated with the prime-and-pull approach. Using Shin and Iwasaki’s strategy, what had been a failed vaccine became an effective treatment.
Then, the pandemic struck. Everything was pushed to one side. Iwasaki’s lab and others around the world leapt into studying the deadly new virus. And right from the beginning, Iwasaki started to hear about the phenomenon that would become her new focus.
Imagine the fear. The illness was bad enough, but everyone says you should be better by now. Instead, every day, you wake up feeling like death: a sign that you’re in uncharted territory. How could you still—four weeks, six weeks, six months after you first got sick—feel this bad? Or maybe you don’t even have to imagine. Maybe you’re one of the 16.3 million working-age Americans with long COVID.
Using the biobank that she began with Albert Ko and others, Iwasaki put out paper after paper in the first months of the pandemic. She and her colleagues reported that people with severe COVID often had a different immune response from the people who got over it more easily. They discovered which immune cells and factors contributed to the lethal disease. They found that men and women had different immune responses to the virus, which helped explain why men seemed to have it worse. They looked at SARS-CoV-2 in the placenta of a patient at Yale New Haven Hospital. Iwasaki’s group was everywhere, and continues to be a juggernaut in understanding what the virus does to those it infects. “I’ve stopped counting high-impact COVID papers” from Akiko, says Mark Coles. “More on the way.”
But she began to hear about the people who did not get better, or, just as alarming, who developed troubling symptoms after even a mild infection. Very early, Ed Yong, a science writer for the Atlantic, brought word of these people to her. “When he asked me to speculate on what the mechanism might be, I thought about it, and then I came up with some hypotheses,” she said. Then she couldn’t stop thinking about it.
Reading Yong’s articles, she learned of David Putrino, a physical therapist and assistant professor at Mount Sinai in Manhattan who was caring for people reporting what we now call long COVID. “Immediately, he said yes to a collaboration,” she said. “He’s an expert in the patient care side. And I’m an expert in the basic science, and we kind of merge our powers together.”
It can be very difficult for people with long COVID to convince others that their suffering is real. Long before the pandemic, people with symptoms similar to those in some cases of long COVID—severe fatigue, brain fog, muscular pain, what is called “rebound fatigue” after trying to do even normal activities—struggled to get acknowledgement. Many were diagnosed with symptoms similar to myalgic encephalomyelitis/chronic fatigue syndrome. Derya Unutmaz, a professor at the Jackson Laboratory who studies ME/CFS, says that in many cases, the disorder was likely triggered by a viral infection. “The problem with ME/CFS was you couldn’t identify the specific virus,” he continues. “With long COVID, it’s so clear.”
Still, to people whose hearts don’t work well after the virus—who have to give up their jobs because they can’t be sure on any given day that they will be able to get out of bed—the fact that Iwasaki believed them right away was a welcome relief. “She is definitely well known in the patient community,” says Hannah Davis, who has long COVID and is a founder of the Patient-Led Research Collaborative, a group that facilitates research on the syndrome.
Over the last two years, Iwasaki, Putrino, and their collaborators have been working to find long COVID’s biomarkers: signs that show up in people with the disorder, but not in healthy people. Finding these markers is the first step to reliably diagnosing long COVID, which likely has multiple forms, and potentially to treating it. In August 2022 the team released a paper on the preprint server medRxiv detailing marked changes in more than 100 people with long COVID.
The list of immune cells and molecules deranged after the body’s brush with the virus is formidable, and heartbreaking. “There are clear biomarkers. These are not just psychological things. There’s real biology to explain them,” says Tianyang Mao ’22PhD, who is involved in the research. “Now is a really good time to really work on this and try to find some answers.”
The study, which is still being peer-reviewed, shows that patients often have signs of an immune system that appears to be failing to control the virus. Perhaps the biggest surprise was that, at least in this relatively small group of patients, long COVID was strongly correlated with low levels of the hormone cortisol. And intriguingly, the patients also have more active antibodies against the Epstein-Barr virus, which causes mononucleosis and stays in the body for life, periodically reactivating itself. “How is that playing into the pathology? Is it playing into the pathology?” asks Alexandra Tabachnikova, a former graduate student on the team.
They are, she says, “trying to figure out why that correlation is there with long COVID, and what could be driving the disease.”
The pandemic brought with it a new notoriety for Iwasaki. She is very active on Twitter these days, answering questions about COVID-19 and long COVID. She’s spoken to the media countless times and recorded videos explaining, in terms anyone can understand, what happens when the virus and the immune system come into conflict.
As she’s risen in prominence, her commitment to a fair, supportive version of the scientific life—her conviction that everyone has a right to see what they can do, as she has done—has not changed. She’s spoken publicly about the precariousness she felt as a young mother and scientist 15 years ago, desperately trying to find care for her children. (She and her husband, Ruslan Medzhitov, also a professor of immunology at the medical school, never managed to get a slot in a campus daycare.)
For young female scientists in her orbit, she is proof that it’s possible to be a mother and also a scientist in the very highest echelons of the field. Mark Coles relates that Jelena Bezbradica Mirkovic, who was a student in Medzhitov’s lab, has spoken often about Iwasaki’s inspiration and support. “I know how much it meant to her, having those discussions with Akiko,” he says. Mirkovic is now an associate professor of immunology at the University of Oxford.
When Ellen Foxman ’93 returned to science after an absence of six years, she found in Iwasaki someone who saw her clearly. “As a woman going back to this very high-powered career trajectory—and having this career hiatus—when I reapproached people after that, I really found that not everybody took me seriously anymore. But I felt that Akiko did. That was huge. I can’t overstate it,” Foxman says. “She understood that I could be a serious scientist and have made the personal choices I made.” Foxman, who holds an MD and a PhD from Stanford, is now head of her own lab at the School of Medicine.
And Iwasaki is genuinely interested in what everyone has to say. Mario Pena-Hernandez, now a graduate student in her lab, remembers approaching her at a reception, after she’d won an important prize. He was just starting out. “The first thing she asked me was, ‘What are you working on?’ She was really curious about my work,” he recalls. “And then we spent the following maybe twenty, twenty-five minutes of the reception talking about flaviviruses. It was really, really fun.”
Perhaps it is this intense awareness of other people that drives Iwasaki’s ability to explain her insights in immunology—an area of biology that has traditionally defied clear description. So many immunology papers are a thicket of what-ifs and highly conditional statements, a dense mess of cell names and signaling pathways that evoke only the system’s complexity, not any collective truths underpinning it.
Some of that thicket reflects the real difficulty of understanding the immune system. But in Mark Coles’s view, the fact that immunology is often poorly communicated, even among scientists, makes it harder to make progress. A paper that is too muddy, he says, can leave you thinking, “If it’s that complicated, is it real?” But Iwasaki has a sense of the principles undergirding the system. She has a way of not only singling those out in her lab’s experiments, but also putting them on the page in a way that will give the reader a glimpse into her vision.
She is aware of you: the audience out there. She is listening.
 loading
loading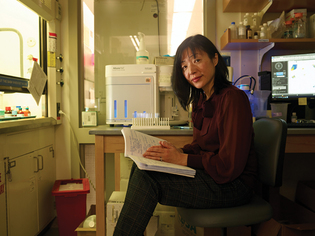
6 comments
-

Benjamin , 5:48pm February 24 2023 |  Flag as inappropriate
Flag as inappropriate
-

Julie Morris, 5:48pm March 01 2023 |  Flag as inappropriate
Flag as inappropriate
-

Angela , 9:58pm March 01 2023 |  Flag as inappropriate
Flag as inappropriate
-

Charmian Proskauer, 2:24pm March 06 2023 |  Flag as inappropriate
Flag as inappropriate
-

Perry Norton, 4:32pm March 06 2023 |  Flag as inappropriate
Flag as inappropriate
-

Luciana Finamor, 7:34am April 02 2023 |  Flag as inappropriate
Flag as inappropriate
The comment period has expired.remarkable, appreciating your invaluable work & science. Thank you.
It is great to hear of such important work that could change the lives of millions for the better. Thank you.
It's so important to keep featuring this urgently needed research. So many people are suffering, gaslit, and in need of hope. Thank you for highlighting the overlap between long COVID and ME!
Excellent article - thank you! Ditto to Angela's comment - the overlap of symptoms between Long COVID, ME/CFS, and other post-acute infectious illness such as post-treatment Lyme disease is strong, and hopefully research on Long COVID will help provide insights and treatments for all of these post-infectious illnesses. It is so inspiring to read about this talented and dedicated researcher.
Thank you for fighting the good fight for all of us...
I am an ophthalmologist researcher from Brazil, and Akiko Iwasaki has inspired me! Her theories about EBV virus gave us many insights and can be also associated with other diseases like ocular Toxoplamosis, and now we are going to study this association! Thanks for all your collaboration! You are going to save lives!